“When you do the math on the study population suffering from intestinal failure; 20% of patients who received a Hickman catheter developed a central-line infection and 18% of those who received a PICC line developed a central-line infection. Polyurethane and silicone PICCs and polyurethane were used for the Hickman lines. Both materials are defective” … Greg Vigna, MD, JD, national product liability attorney.
What did Lars Vinter-Jensen say in the study “Comparison of complications associated with peripherally inserted central catheters and Hickman catheters in patients with intestinal failure receiving home parenteral nutrition. Six-year follow-up study” in Clinical Nutrition 35 (2016) 912-917?
“The clinical features vary greatly depending on the function and length of the remaining bowel. When the condition is permanent it is defined as chronic intestinal failure.
The mean time to first catheter-related bloodstream infection was significantly shorter for PICCs compared to Hickman catheters (84 vs. 297 days)
The incidence of catheter-related bloodstream infection per 1000 catheter days was significantly lower for Hickman catheters when compared to PICCs ( 0.56 vs. 1.63).
A total of 75 catheters were removed due to catheter-related bloodstream infection, 49 Hickman catheters and 26 PICCs respectively.
We found a higher risk and shorter time to first catheter-related bloodstream infection in PICCs compared to Hickman catheters supporting that PICCs should mainly be chosen for planned home parenteral nutrition up to 3-6 months.
Read the above study: https://www.sciencedirect.com/science/article/pii/S0261561415001879
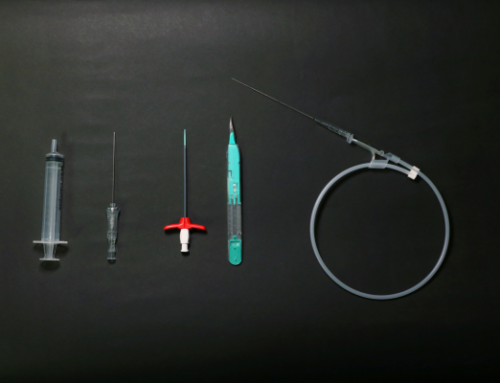
Greg Vigna, MD, JD, national product liability attorney, PICC line and midline attorney states, “Patients are being discharged on home nutrition by vein, also referred to as total parenteral nutrition or TPN, by way of PICC lines, ports, and tunneled catheters. The most common serious complications are line sepsis and blood clots. Polyurethane and silicone tubing that goes into the veins do little to nothing to reduce the risk of these serious complications and there are safer materials available for patients.”
Dr. Vigna concludes, “Patients with intestinal failure should not be exposed to polyurethane and silicone venous access devices because they don’t have the hydrophilic qualities that reduce bacterial colonization and platelet aggregation that reduce the risks of infection and blood clots. This study shows that approximately 20% of those with intestinal failure developed a bloodstream infection. That is brutal and profits over patient safety is not acceptable.”
Dr. Vigna is a California and Washington DC lawyer who represents those with serious injuries caused by defective medical devices. He represents the injured with the Ben Martin Law Group, a national pharmaceutical injury law firm in Dallas, Texas. The attorneys are product liability and medical malpractice attorneys, and they represent the most injured across the country.
Resources:
https://www.birpublications.org/doi/full/10.1259/bjr/32639616
https://www.tandfonline.com/doi/abs/10.1080/17434440.2019.1555466
https://www.sciencedirect.com/science/article/pii/S0261561408000757