“The standard of care for management of deep Stage III and Stage IV decubitus ulcers includes the plastic surgery component. These are serious injuries and outcomes are bad without access to myocutaneous flaps” … Greg Vigna, MD, JD, national decubitus ulcer attorney, Board Certified Physical Medicine and Rehabilitation.
Dr. Anke Scheel-Sailer, MD, Spinal Cord Medicine, Swiss Paraplegia Foundation describes the “multimodal treatment concepts connecting acute and rehabilitation care” to the management of Stage III or Stage IV decubitus ulcers in her article, “Treatment and cost of pressure injury stage III or IV in four patients with spinal cord injury: the Basel Decubitus Concept” in Spinal Cord Series and Cases (2019) 5:30:
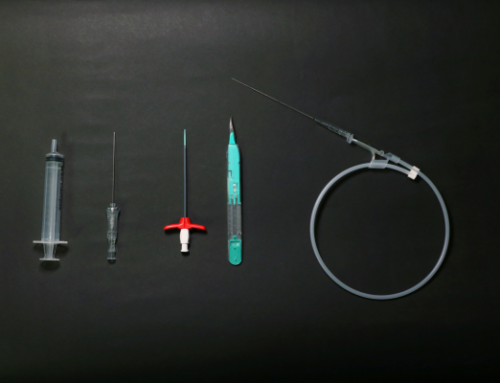
“The modified ‘Basel Decubitus Concept’ includes the following relevant single intervention components and relevant milestones.
To learn more about Dr. Scheel-Sailer’s article: https://www.nature.com/articles/sc2013130
Dr Vigna states, “Unfortunately, the standard of care appears to be far and far between for people who suffer deep Stage 3 and Stage 4 decubitus ulcers. The injured require the standard of care after injury and that appears to be a scarce resource. That needs to change.”
Dr. Vigna Explains the Basel Decubitus Concept: (Part 1)
Pressure relief must be reliable for those with one or more deep Stage III or Stage IV decubitus ulcers, and I preferred clinitron beds as they provide reliable pressure relief. Infection control and wound conditioning are best provided by surgical debridement of infected and non-viable tissue in the operating room and IV antibiotics are provided if there is local or systemic infection. The surgical debridement must be provided to get the wound bed ready for closure. All necrotic tissue and undermining must be debrided to viable tissue. Then, local wound care is best provided with Kerlix dressing once or twice a day. VAC packs can also be used. Nutritional optimization and other medical treatments must be provided as these people are sick and need to be medically optimized before major surgery and optimizing a patient will improve outcomes. We ordered PEG tubes for those with nutritional requirements that are not being maintained by mouth. Spasticity may need to be treated and diabetic control should be optimized. None of these patients were allowed to smoke.
Dr. Vigna concludes, “Once patients are medically optimized, the wound is free of necrotic tissue and infection, with evidence of granulation tissue developing they are ready for plastic surgery.”
To learn about health outcomes of patients with deep Stage III or Stage IV decubitus ulcers read: https://journals.sagepub.com/doi/full/10.1177/20499361231196664
Greg Vigna, MD, JD, is a national malpractice attorney and an expert in wound care. He is available for legal consultation for families and patients who have suffered decubitus ulcers because of poor nursing care at hospitals, nursing homes, or assisted living facilities. The Vigna Law Group along with Ben C. Martin, Esq., of the Martin Law Group, a Dallas Texas national pharmaceutical injury law firm, jointly prosecute hospital and nursing home neglect cases that result in bedsores nationwide.
To learn more: https://vignalawgroup.com/decubitus-ulcer-help-desk/