DECUBITUS ULCER
What Are Decubitus Ulcers?
Also known as pressure ulcers or bedsores, decubitus ulcers are areas of skin and underlying tissue damage that occur due to prolonged pressure on the skin. These ulcers are caused by sustained pressure, friction, or shear and can vary in severity from mild reddening of the skin to severe tissue damage that can affect muscles and bones.
How Do You Get Decubitus Ulcers?
Decubitus ulcers develop when prolonged pressure on the skin impairs blood flow to the area. This can occur in several situations, particularly in individuals who have limited mobility like those in nursing homes or longer term care facilities.
OUR CREDO
“Holding hospitals and nursing homes accountable, while our clients obtain the care they deserve.” Greg Vigna, MD, JD, national malpractice attorney
In 2006, the Centers for Medicare & Medicaid Services identified pressure ulcer prevention as a nursing quality indicator and full-thickness pressure ulcers were deemed “never events.” CMS defined never events as preventable medical errors that result in serious consequences for the patient and unnecessary treatment costs.
“Never Events” are errors in medical care that indicate a real problem in safety and credibility of a healthcare facility. Included on the list of “Never Events,” decubitus is surgery on the wrong body part, leaving a surgical instrument in a patient after surgery, major medication errors.
1. Unambiguous
2. Usually preventable
3. Serious resulting in death or loss of a body part, disability, or more than a transient loss of a body function
4. Indicative of a problem in a health care facility’s safety system and is important for public credibility or public accountability
The law requires hospitals and nursing homes to investigate each event, report its underlying cause, and take corrective actions to prevent similar events. “Never Events” can be eliminated by providing increased resources and education of hospital and nursing home staff.
CONTACT US FOR A FREE CONSULTATION
“Hospitals and nursing homes know how to point the finger at other providers and many times will point the finger back at the patient and their families. The only path to change is by punishing them financially and taking depositions of those who are responsible. We do our own investigation for the benefit of our clients and future patients of the negligent healthcare facility. Don’t be fooled by being told it is a Grade I Decubitus Ulcer.”
Greg Vigna, MD, JD, national malpractice attorney
Pressure Sore Staging and Staging of Decubitus Ulcers
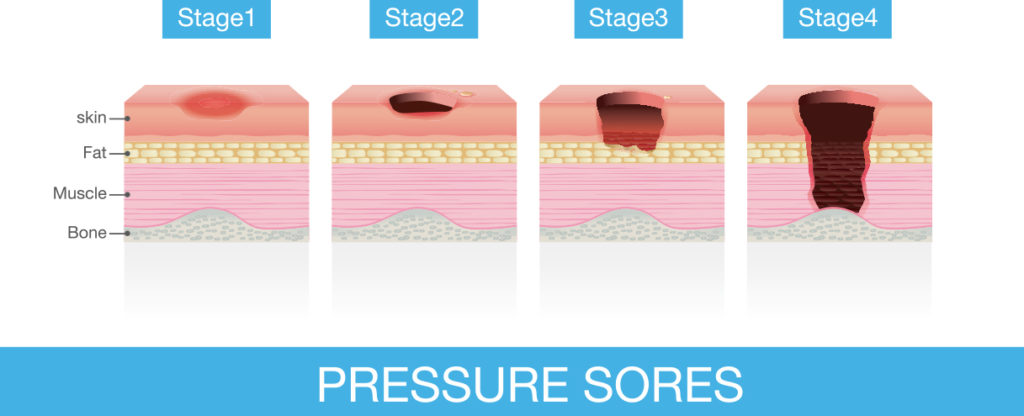
Decubitus ulcer classification is primarily visual but may be by palpation. There are four
stages (I-IV) but it must be understood that a Stage I decubitus ulcer may have a deep tissue
component not yet visible on clinical exam. Suspected deep tissue injury would include
subcutaneous bruising suggestive of a Grade III-IV decubitus ulcer.
Stage I: Non-blanchable redness over a bony prominence
Stage II: Partial dermis loss
Stage III: Full thickness tissue loss
Stage IV: Full thickness tissue loss with exposed bone, tendon, or muscle
Proper off-loading:
Ex. Stage I sacral decubitus: Requires side to side lying with the head of bed not higher than 30 degrees.
Ex. Stage III sacral decubitus: Requires side to side lying with the head of bed not higher than 30 degrees.
If adequate pressure relief cannot be obtained because of patient related factors that might include pain or multiple decubitus ulcers, patients require a clinitron bed to ensure absolute off-loading of the bed sore or sores.
Ex. Ischial decubitus ulcer: Off-loading either requires no sitting, or if superficial decubitus ulcer is confirmed, limited sitting with adequate pressure reliefs every ten minutes.
Populations at Risk:
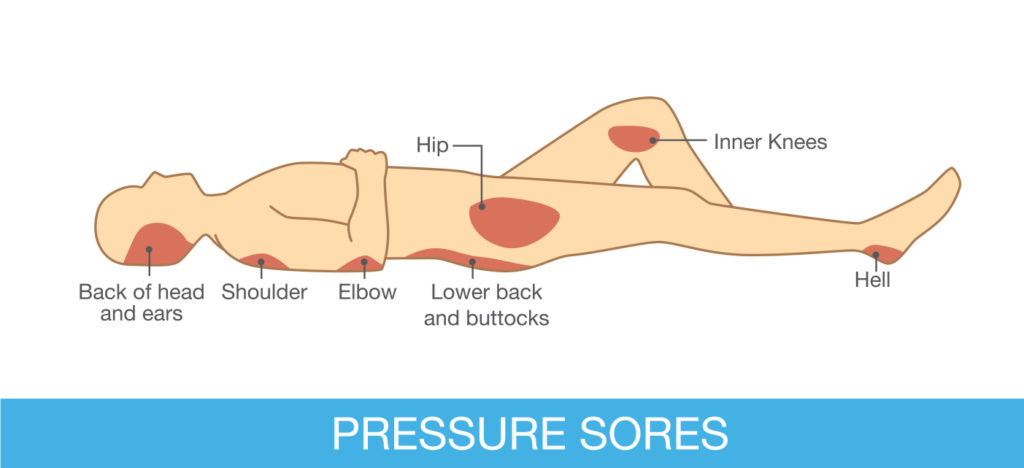
- Nursing home residents
- Dependent patients in transit from one facility to another
- Spinal cord injured patients
- Critically ill patients
Multidisciplinary Approach to Management of Grade III & Grade IV Decubitus Ulcers
Patients with Grade III and Grade IV decubitus ulcers are medically complex. They tend to be debilitated, malnourished, and are often septic. These patients require a level of care that allows for a multitude of services and time to heal. A Long-Term Acute Care (LTAC) facility has a licensure that allows for patients to stay one to two months.
“Decubitus ulcers are either superficial or deep. Superficial decubitus ulcers are injuries to the skin and adjacent soft tissues are generally caused by shear forces that essentially pull on the skin. Deep tissue injuries are on the other hand are caused by pressure from inadequate turning or incomplete pressure reliefs that leads to irreversible damage and death of the muscles induced by a loss of blood flow from pressure on the arterial supply to muscle cells.” Greg Vigna, MD, JD, national malpractice attorney
“Populations at risk haven’t changed overtime as those at risk all have impairments in mobility because of disability or acute medical illnesses. What has changed over the past two decades is the quality of care at the bedside in hospitals and nursing homes across the country. Resources have been diverted from patient care to non-essential expenses that include dividend payments to shareholders and inflated allocations to hospital administrations who aren’t being held accountable for the errors within the walls of the facilities that they oversee.” Greg Vigna, MD, JD, national malpractice attorney
IN THE NEWS…
Management of Deep Tissue Injuries in Patients at Risk for Pressure Injuries
“Most commonly, deep tissue pressure injuries appear on the skin over the coccyx or sacrum, the buttocks, and the heel,” states Ave Preston, RN, CWOCN, University of Pennsylvania Hospital. Greg Vigna, MD, JD, national pressure [...]
Kindred Hospital Philadelphia-Havertown Hit with Bedsore Wrongful Death Lawsuit
“Our client suffered a serious Stage IV pressure injury and was transferred to Kindred Hospital Philadelphia-Havertown. We allege our client was then not provided effective care and lost an opportunity for cure when he was [...]
Daleview Care Center Hit with ‘Never Event’ Bedsore Lawsuit
“We represent those who have hospital acquired Stage III or Stage IV bedsores that are discharged to nursing homes without being offered the standard of care recommended by Wound Healing Society Guidelines. Early flap closure [...]
TEAM MEMBERS
Plastic Surgery: Surgical debridement & Musculocutaneous Flaps
A plastic surgeon is an essential member of a multidisciplinary team, as they have the skills to provide surgical debridement and musculocutaneous flaps.
Surgical debridement is a mainstay of treatment of Grade III and IV decubitus ulcers. Grade III and Grade IV decubitus ulcers that have necrotic tissue with or without infection will not heal. Essential management is early surgical debridement to viable tissue, which is medically necessary as wounds will not heal if dead tissue remains in the wound base.
Musculocutaneous flaps is a mainstay of treatment of Grade III and IV decubitus ulcers once there is a stable wound base, nutrition of a patient is optimized, and infection has been treated. Surgical options for flap closure depend on the location of the wound. The most common locations are below, understanding that with virtually any location on the body, there are options for closure:
Physical Medicine & Rehabilitation with or without Internal Medicine
A Physical Medicine and Rehabilitation physician, who is trained in the management of Grade III and IV decubitus ulcers is necessary for the management of a medically complex patient, with or without the assistance of an Internal Medicine Physician. These physicians will need to direct care as it relates to treatment of soft tissue infections, including osteomyelitis (bone infection), nutritional support, selecting the most appropriate bed to allow for guaranteed pressure relief, directing the wound care as it relates to dressing changes, treatment of anemia, and supervising the rehabilitation team at the time when patients can be safely mobilized out of bed.
Orthopedic Surgeons
Complex wounds may have old, chronically infected hardware from remote surgeries that may need to be removed. Patients may have extremities that are not salvageable, and amputations may be necessary. Septic joints may require incision and drainage at the time of surgical debridement. Chronic osteomyelitis may require extensive bone debridement and there may be a need for surgical placement of antibiotic beads into the freshly debrided bone at the time of flap closure of a large wound involving the pelvis.
Nursing Wound Care
Nurses trained in the post-operative management of flaps are imperative to prevent complications. Management of surgical drains and proper turning techniques is necessary to avoid failure of a flap because of a post-operative hematoma or undue tension at the incision site during a patient turn.
Physical and Occupational Therapy
Post-flap management requires therapists who are trained in safe sitting programs following flap closure and the gradual mobilization of patients as they begin the process of rehabilitation to allow for a safe discharge to home or a lower level of care.
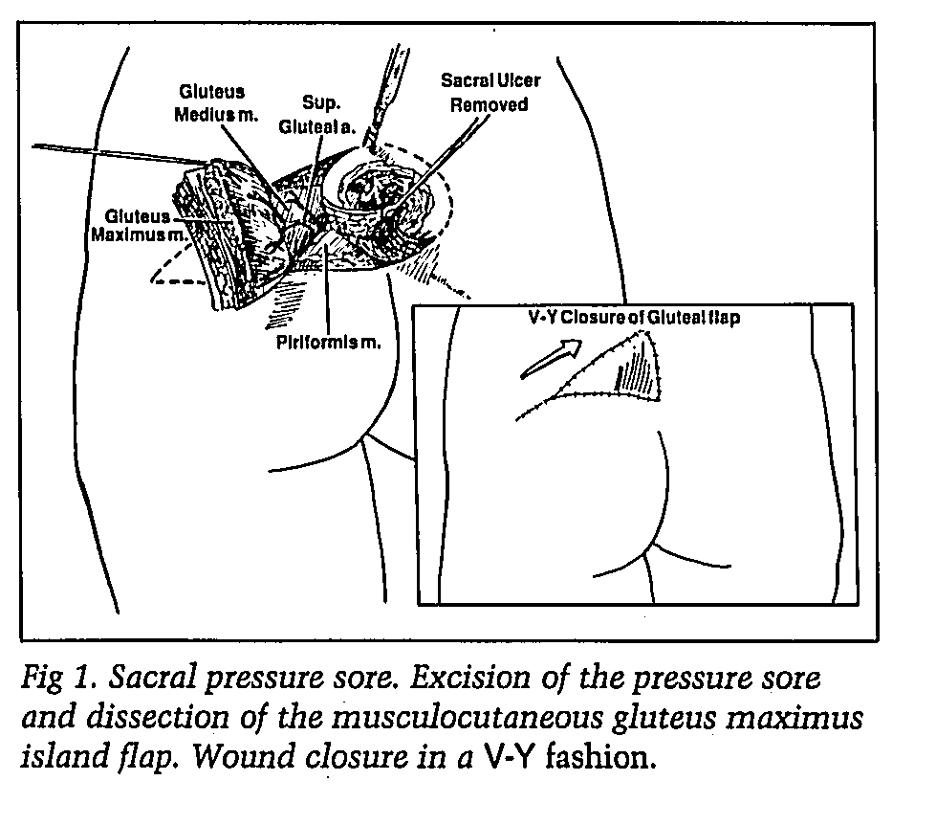
Sacral decubitus ulcers: Gluteus maximus musculocutaneous flap
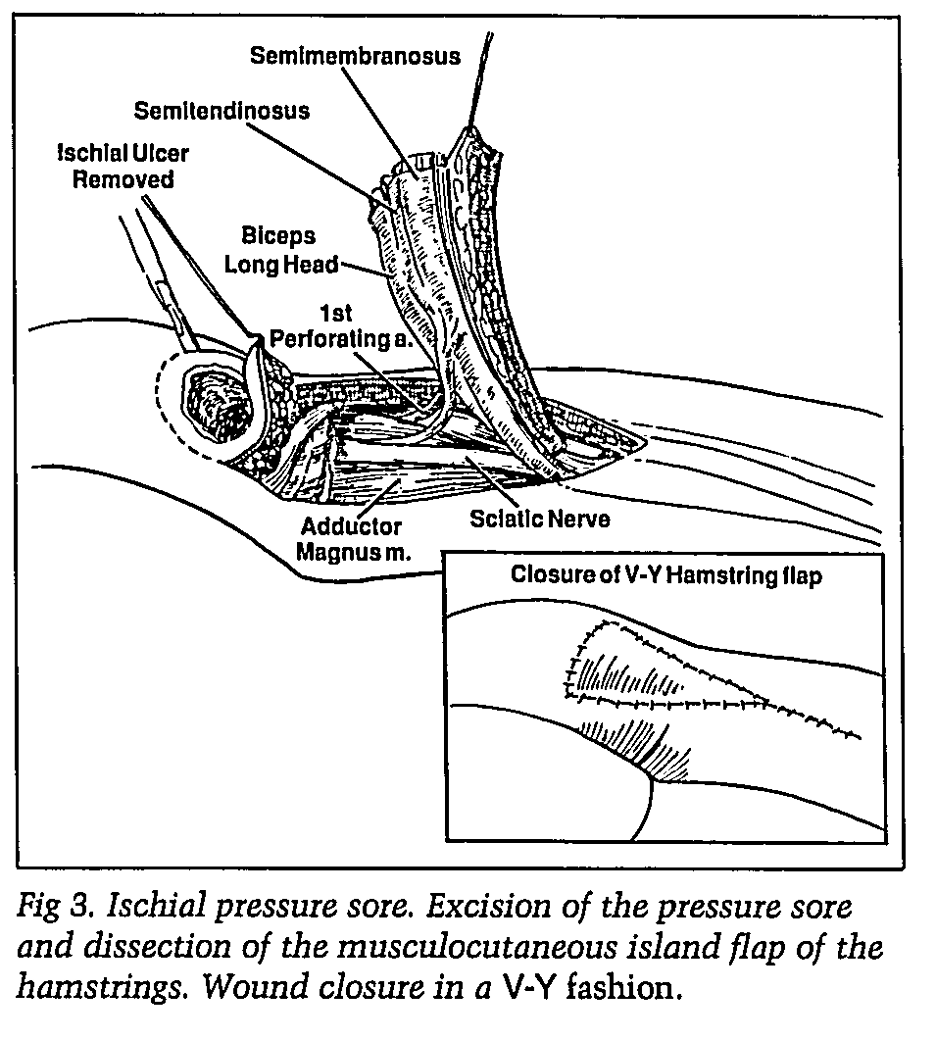
Ischial decubitus ulcer: Hamstring flap/Gluteus maximus flap
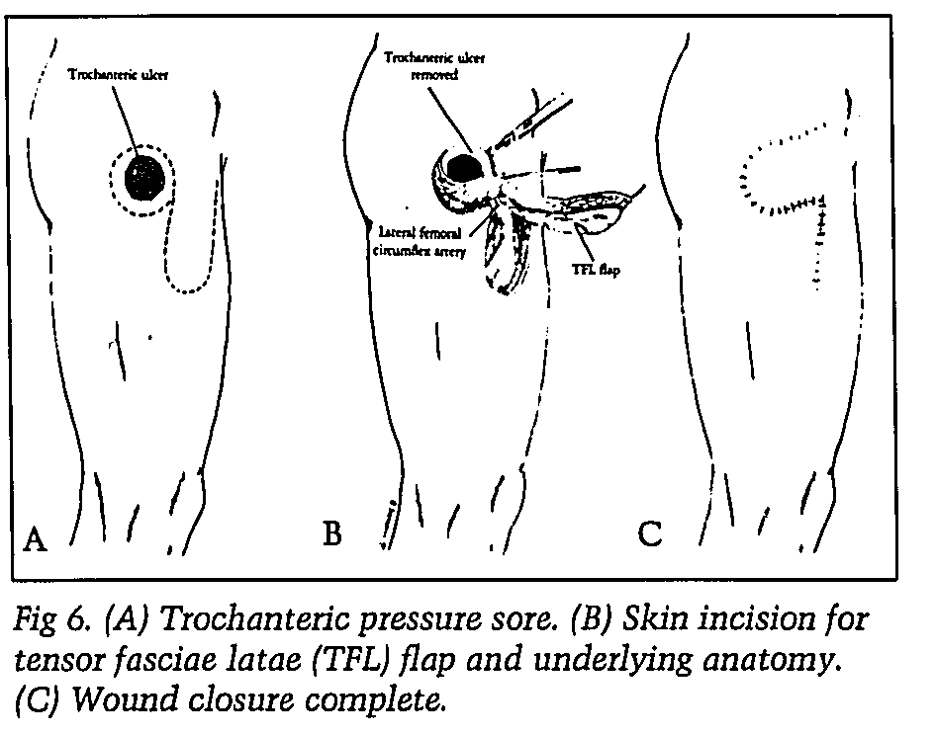
Trochanter: Tenor fasciae latae flaps
Grade III or Grade IV decubitus ulcer

This is a Grade III or Grade IV decubitus ulcer. Depth is unknown at this time as there is a central area of necrosis that may extend to bone. Treatments may include any of the following:
- Nutritional support that may include oral supplements if patient can tolerate by mouth
- Surgical debridement in the operating room or bedside
- IV antibiotics if purulent drainage is noted at the time of debridement
- Pressure relief, side to side turns every two hours
- Air mattress
- Flap closure or VAC pack if this is a deep Grade III/IV after wound is stable without infection or necrotic tissue
This is a Grade III decubitus ulcer. This ulcer should heal with proper pressure relief and ongoing conservative wound care or can be closed with a musculocutaneous flap.
Grade III decubitus ulcer

Grade III, possible Grade IV decubitus ulcer

This is a Grade III, possible Grade IV decubitus ulcer that has necrotic tissue and might be infected. This wound requires debridement in the operating room or at bedside with appropriate local anesthesia. Wound culture at the time of debridement should likely be obtained.
This is a Grade IV sacral decubitus ulcer, and this wound is not compatible with life. Options will include hospice care versus aggressive care that would include any or all of the following:
1) Surgical Debridement
2) Clinitron Bed
3) PEG placement for nutritional support
4) IV antibiotics
5) Prolonged conservative wound care until nutrition is optimized, then flap closure
Grade IV sacral decubitus ulcer