And what causes them?
Also called pressure ulcers or bedsores, decubitus ulcers result from prolonged pressure that damages the skin and underlying tissues. These injuries can range from mild skin redness to severe wounds exposing muscle or bone. Friction and shear forces also contribute.
Prolonged pressure cuts off blood flow, damaging tissue. These ulcers are most common in patients with limited mobility—especially in hospitals, rehabilitation facilities, and nursing homes.
Accountability in Care
“Holding hospitals and nursing homes accountable for the injuries they cause and the ineffective care they provide”
—Greg Vigna, MD, JD, National Malpractice Attorney
Healthcare facilities are legally obligated to investigate and report ’Never Event’ pressure injuries and to ensure that patients who are dependent on caregivers for repositioning receive the bedside care they require.
Decubitus Ulcers deemed as “Never Events” by the Centers for Medicare & Medicaid Services (CMS)
Never Events Defined:
- Clear and preventable
- Result in death, disability, or serious injury
- Reflect systemic safety failures
- Demand full transparency and corrective action
Healthcare facilities are legally obligated to investigate, report, and resolve the causes of these events. Proper staff education and increased resources can prevent them.
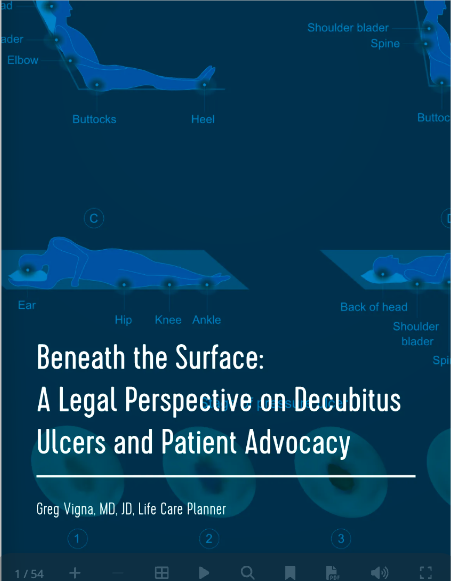
Understanding Pressure Ulcer Stages
- Stage I: Redness over a bony area that doesn’t blanch
- Stage II: Partial skin loss
- Stage III: Full-thickness tissue loss
- Stage IV: Full-thickness loss with exposed bone, tendon, or muscle
Deep Tissue Injuries Can Be Hidden
Bruising or skin discoloration may signal deeper tissue death. These injuries often declare themselves as Grade III or IV ulcers weeks later. Reliable, scheduled skin checks and consistent pressure relief are essential.
Proper Off-Loading Techniques
- Stage I sacral ulcer: Side-to-side turning, bed angle below 30°
- Stage III sacral ulcer: Same protocol, plus specialized beds if pain or multiple ulcers exist
- Ischial ulcer: No sitting, or limited sitting with pressure relief every 10 minutes
Who’s at Risk?
- Nursing home residents
- Hospitalized or immobile patients
- Individuals with spinal cord injuries
- Critically ill or medically complex individuals
Management of Grade III & IV Ulcers
Patients with advanced ulcers often face infection, malnutrition, and systemic illness. These cases demand care in Long-Term Acute Care (LTAC) hospitals, where they can receive sustained, multidisciplinary treatment.
Treatment Must Be Aggressive
“Muscle is more vulnerable than skin. By the time surface damage is visible, irreversible harm is often done underneath. Within 2–3 weeks, a small wound can become a gaping hole.”
—Greg Vigna, MD, JD
Medical Failures Behind Deep Tissue Injuries
These injuries occur when staff fail to reposition dependent patients. Lying patients must be turned every 2 hours; seated patients need relief every 15–20 minutes. Anything less is unacceptable and dangerous.
Multidisciplinary Treatment Is Essential
- Plastic Surgeons: Perform surgical debridement and flap closures
- Physiatry/Internal Medicine: Manage infections, anemia, and nutrition; direct rehab
- Orthopedic Surgeons: Remove infected hardware, address bone involvement
- Wound Nurses: Handle drains and manage incisions post-flap
- Physical/Occupational Therapists: Guide safe mobilization after surgery
Examples of Surgical Options
- Ischial ulcers: Hamstring or gluteal flaps
- Sacral ulcers: Gluteus maximus flap
- Trochanteric ulcers: Tensor fasciae latae flaps
Critical Stage IV Cases
Some wounds—like a Stage IV sacral ulcer with necrosis to the bone—may not be survivable. Families must weigh hospice versus aggressive intervention, which may involve:
- Surgical debridement
- Clinitron bed
- Nutritional PEG tube
- IV antibiotics
- Pressure relief until flap surgery becomes viable